Efficacy
In the ELIANA trial, the majority of KYMRIAH patients attained and sustained remission
A potentially definitive treatment
ELIANA Study Design
Study characteristics of the global, phase 2 pivotal trial1,2
ELIANA was an open-label, multicenter, single-arm, global phase 2 trial of tisagenlecleucel in 79 patients with B-cell ALL who were primary refractory, chemorefractory, relapsed after, or were not eligible for allogeneic SCT (NCT02228096).
ELIANA Baseline Characteristics
Inclusion/Exclusion Criteria2
Inclusion:
— r/r B-cell ALL, aged 3-21 yearsa
— Bone marrow with ≥ 5% lymphoblastsExclusion:
— Isolated extra-medullary disease relapse
— Prior CD19-directed or gene therapy
End Points1
Primary: Overall remission rate (CR/CRi) within 3 months after infusion1
— 4-week maintenance of remission
— IRC assessmentSecondary: CR or CRi with MRD-negative bone marrow, DOR, OS, EFS, cellular kinectics, safety1
aAge of 3 years at the time of screening to age 21 years at time of initial diagnosis.1
PRIOR ANALYSIS 2,3 | ASH 2018: 24 MONTHS1 | |
USPI: 4.8 MONTHS (N=63)2
| Based on: 79 INFUSED PATIENTS
| Type of disease 8% PRIMARY 92% RELAPSED DISEASE
|
ALL, acute lymphoblastic leukemia; ASH, American Society of Hematology; CR, complete remission; CRi, complete remission with incomplete blood count recovery; DOR, duration of remission; EFS, event-free survival; IRC, Independent Review Committee; MRD, minimal residual disease; NEJM, New England Journal of Medicine; OS, overall survival; SCT, stem cell transplant; USPI, United States Prescribing Information.
ORR and MRD-Negative Remission
WITH KYMRIAH, THE MAJORITY OF PATIENTS ATTAINED AND SUSTAINED MRD-NEGATIVE REMISSION1
About 8 out of 10 patients achieved MRD-negative remission at 3 months after treatment with KYMRIAH® (tisagenlecleucel).1 MRD-negative status is a strong marker for positive prognosis.4
bORR consisted of complete remission (CR) and complete remission with CRi, defined as less than 5% of blasts in the bone marrow, no evidence of extramedullary disease, and without full recovery of peripheral blood counts with or without blood transfusion). Remission status was required to be maintained for at least 28 days without clinical evidence of relapse.2
cMRD-negative was defined as MRD by flow cytometry <0.01%.2
dFive patients who were infused with KYMRIAH were excluded from the efficacy set in the interim analysis. The efficacy analysis set (n=63) is a subset of the full analysis set (N=68), which consisted of all patients treated with KYMRIAH at least 3 months prior to data cutoff.2
eDay 28 assessment initially defined as ±7 days; definition changed to ±4 days after 1 site was enrolled, 3 patients were enrolled, and 1 patient was treated.5
REMISSION WAS ACHIEVABLE WITH KYMRIAH REGARDLESS OF CLINICAL CHARACTERISTICS5,6
KYMRIAH demonstrated consistent response rates across all subgroups evaluated, including high-risk patient subgroups
NR, not reported.
fFive patients who were infused with KYMRIAH were excluded from the efficacy set in the interim analysis. The efficacy analysis set (n=63) is a subset of the full analysis set (N=68), which consisted of all patients treated with KYMRIAH at least 3 months prior to data cutoff.2
gThe area of each box is proportional to the number of patients in the particular grouping. The 95% CIs are exact Clopper-Pearson CIs calculated for each subgroup.5
hIncludes 8 patients categorized with chemorefractory disease at study entry.6
RFS and OS
KYMRIAH DELIVERS DURABLE RESPONSES IN PATIENTS WITH R/R ALL (≤25 YEARS)1
Median relapse-free survival (RFS) was not reached at 24 months1
iRFS was defined as time since onset of CR or CRi to relapse or death due to underlying cancer, whichever is earlier, censoring for new cancer therapy, including SCT.3
USPI: 4.8 MONTHS6
As reported in the USPI at 4.8 months after response, 75% of responders were estimated to still be in remission at 6 months, and 64% of responders were estimated to still be in remission at 9 and 12 months.6
KYMRIAH Persistence Based on Pharmacokinetics2
KYMRIAH was present in the blood and bone marrow and was measurable beyond 2 years.
TWO-THIRDS OF PATIENTS TREATED WITH KYMRIAH WERE ALIVE AT 2 YEARS1
Median OS was not reached at 24 months1
OS was a secondary efficacy end point of the global phase 2 pivotal trial1
OS data are not in the Prescribing Information and should be interpreted with caution in a single-arm trial. The statistical significance of OS is not known
NE, not evaluable.
STEM CELL TRANSPLANT AFTER KYMRIAH DOES NOT APPEAR TO IMPROVE OVERALL SURVIVAL3,7
At a median follow-up of 13.1 months postinfusion, 87% of responders did not proceed to SCT.
No difference in OS was observed between the full patient population (including the 13% of patients who underwent SCT while in remission after KYMRIAH infusion) and those who did not receive SCT.
OS was a secondary efficacy end point of the global phase 2 pivotal trial1
OS data are not in the Prescribing Information and should be interpreted with caution in a single-arm trial. The statistical significance of OS is not known
Patient-reported QOL
PATIENTS REPORTED INCREASES IN QUALITY-OF-LIFE MEASURES AFTER KYMRIAH INFUSION8
KYMRIAH led to a decrease in severity of problems at Months 3 and 6 compared with baseline as assessed via the EQ-5D questionnaire.8
The quality of life study is not part of the Prescribing Information. The PedsQL, EQ VAS, and EQ-5D models were evaluated and validated in a patient population that did not include patients with pediatric ALL. The patient population decreased over time. The study’s statistical significance was not evaluated and, therefore, should be interpreted cautiously.
IMPROVEMENTS IN QUALITY OF LIFE9
MOBILITY
SELF-CARE
ANXIETY/DEPRESSION
USUAL ACTIVITIES (eg, returning to school)
PAIN/DISCOMFORT
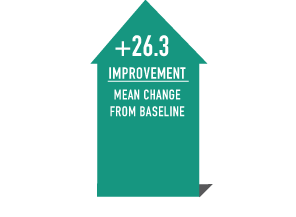
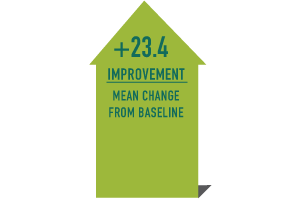
QUALITY-OF-LIFE IMPROVEMENTS WERE OBSERVED AS EARLY AS 3 MONTHS AND SUSTAINED THROUGH 12 MONTHS AFTER KYMRIAH INFUSION9,j
PedsQLTMk
(Pediatric QOL Inventory; baseline n=43)
The minimal change considered clinically
important in the PedsQL questionnaire is 4.4
(for self reports; 4.5 for proxy reports)5,10
EQ-5D VALl
(EQ VAS; baseline n=40)
The minimal change considered clinically
important in the EQ VAS questionnaire is 7 to 1011
EQ-5D, EuroQol 5 Dimension; EQ VAS, EuroQol Visual Analogue Scale; PedsQL, Pediatric Quality of Life Inventory; QOL, quality of life.
j107 patients were screened for the ELIANA trial between April 8, 2015, and April 25, 2017; 92 were enrolled, 75 received KYMRIAH, and 58 were aged 8 to 23 years and included in the analysis displayed here. Tumor response was evaluated on Day 28, every month, to Month 6, then every 3 months until Month 12. Patients are being followed for efficacy and safety for 5 years unless withdrawn from study by patient or investigator choice or lost to follow-up. The data shown are from the mixed model analysis.8
kThe 23-item PedsQL addresses the physical, emotional, social, and school functioning of healthy children and children with chronic disease (scale, 0‐100).8,10
lThe EQ-5D includes questions on the 5 dimensions of mobility, self-care, usual activities, pain/discomfort, and anxiety/depression and a VAS that records self-rated overall health state (range, 0-100).8,11
Supporting Trial: CHP 959
CHP 959 study characteristics12,13
CHP 959 was an open-label, single-site, phase 1/2, supportive, proof-of-concept study of KYMRIAH in pediatric and young adult patients with r/r B-cell precursor ALL (N=62) initiated by the University of Pennsylvania in 2012. These data were not included in the KYMRIAH Prescribing Information12
Enrolled patients aged 1-24 years (median, 11 years)12
Primary end point: Safety, feasibility, and duration of CAR-T cells in vivo12,m
Secondary end point: Anti-tumor activity, including13:
— Day 28 ORR (CR + CRi)
— DOR (from the date of CR/CRi to relapse or death due to underlying cancer)There were some differences noted between this study and the pivotal ELIANA study, and results should be interpreted with caution
CHP 959 COHORTS (N=62)12 | NON-CNS3 ALL COHORTS (N=56)12 | |
Three cohorts:
All the patients infused | Type of disease:
| 57% of patients had high baseline disease burden (≥5% blasts)
|
CNS, central nervous system.
mDetermined via reverse transcriptase-polymerase chain reaction (RT-PCR) analysis of whole blood.12
Safety results from CHP 95914
The majority (89.3%) of patients with non–CNS3 ALL in CHP 959 experienced at least 1 serious adverse event any time after CTL019 infusion. The most common (incidence ≥20%, all grades) serious adverse events regardless of study drug relationship were CRS (82.1%), febrile neutropenia (71.4%), hypotension (39.3%), encephalopathy (26.8%), and pyrexia (23.2%). The most common (incidence >30%, all grades) adverse events regardless of study drug relationship in the non–CNS3 ALL group were decreased white blood cell count (WBC; 94.6%), decreased hemoglobin (92.9%), decreased neutrophil count (91.1%), CRS (89.3%), decreased platelet count (87.5%), lymphopenia (82.1%), febrile neutropenia (78.6%), vomiting (78.6%), aspartate aminotransferase (AST) increased (75.0%), headache (75.0%), nausea (75.0%), alanine aminotransferase (ALT) increased (71.4%), decreased appetite (69.6%), hypogammaglobulinemia (66.1%), diarrhea (57.1%), cough (55.4%), hypotension (51.8%), pain (48.2%), tachycardia (46.4%), fatigue (44.6%), chills (39.3%), increased blood creatinine (35.7%), pyrexia (35.7%), activated partial thromboplastin time prolonged (33.9%), hyperphosphatemia (33.9%), and abdominal pain (32.1%). The most frequently reported (in at least 30% of patients) grade 3/4 adverse events by preferred term (PT), regardless of study drug relationship, were febrile neutropenia (78.6%), decreased neutrophil count (69.6%), lymphopenia (67.9%), decreased WBC count (62.5%), decreased platelet count (48.2%), CRS (46.4%), decreased appetite (35.7%), hypotension (32.1%), decreased hemoglobin (30.4%), and increased ALT (30.4%).
Primary End Point: Safety in Non-CNS3 ALL Patients (N=56)
Nonhematological adverse events | All grades (%) |
Cytokine release syndrome | 91 |
Febrile neutropenia | 80 |
Vomiting | 79 |
Headache | 75 |
Nausea | 75 |
Decreased appetite | 70 |
Cough | 57 |
Diarrhea | 57 |
Hypotension | 52 |
Pain | 48 |
Tachycardia | 48 |
Fatigue | 45 |
Chills | 41 |
Pyrexia | 36 |
Abdominal pain | 32 |
Secondary End Point
REMISSION RATES BY BASELINE DISEASE BURDEN (N=60)14
CR, complete response.
nMRD-negative was defined as MRD by flow cytometry <0.01%.15
Patients Responded to Treatment With CTL019, Across Disease Characteristics15
Data presented here are based on a different analysis of CHP 959 with a population of 60 patients
CNS INVOLVEMENT (N=60)14
CNS status at infusion | Patients, n (%) |
CNS1 | 54 (90) |
CNS2o | 4 (7) |
CNS3p | 2 (3) |
CNS3p within 12 months of infusion | 16 (27) |
oCNS2 status defined as blast cells detected in a sample with <5 leukocytes per cubic millimeter and <10 erythrocytes per cubic millimeter.16
pCNS3 status defined as blast cells detected in a sample with ≥5 leukocytes per cubic millimeter and <10 erythrocytes per cubic millimeter.16
Remission Rates by CNS Status15
Experience with KYMRIAH in patients with active CNS leukemia is limited, and these data should be interpreted with caution
CHP 959 COHORTS (n=60)15 | ANY PRIOR CNS DISEASE (n=11/15)15 | CNS2 OR CNS3 (n=5/6)15 |
No CNS relapses
| 73%of evaluable patients with prior CNS disease (n=11/15) achieved continuous remission as long as 2.5 years | 83%of patients with CNS2 or CNS3 status at infusion (n=5/6) achieved CNS remission |
Persistence Based on Pharmacokinetics15
98% of all patients treated had detectable levels of CTL019 in cerebrospinal fluid (CSF), with lumbar puncture showing detectable CTL019 at 1 year